Surgery for lung cancer

The aim of curative surgery is to remove the part of your lung containing the tumour and any nearby lymph nodes.
Types of surgery
The type of surgery you have will depend on the size of the tumour, where it is and your general health. The main types of surgery are:
Lobectomy: Removal of a lobe of your lung. The removal of 2 lobes of your lung is called a bi-lobectomy.
Pneumonectomy: Removal of your entire lung. Your surgeon will usually remove lymph nodes near the tumour, as this is where the cancer will usually spread to first.
Sometimes patients worry they will be unable to breathe properly after surgery. Your surgeon will assess this beforehand to ensure that you will still be able to breathe properly with just one lung.
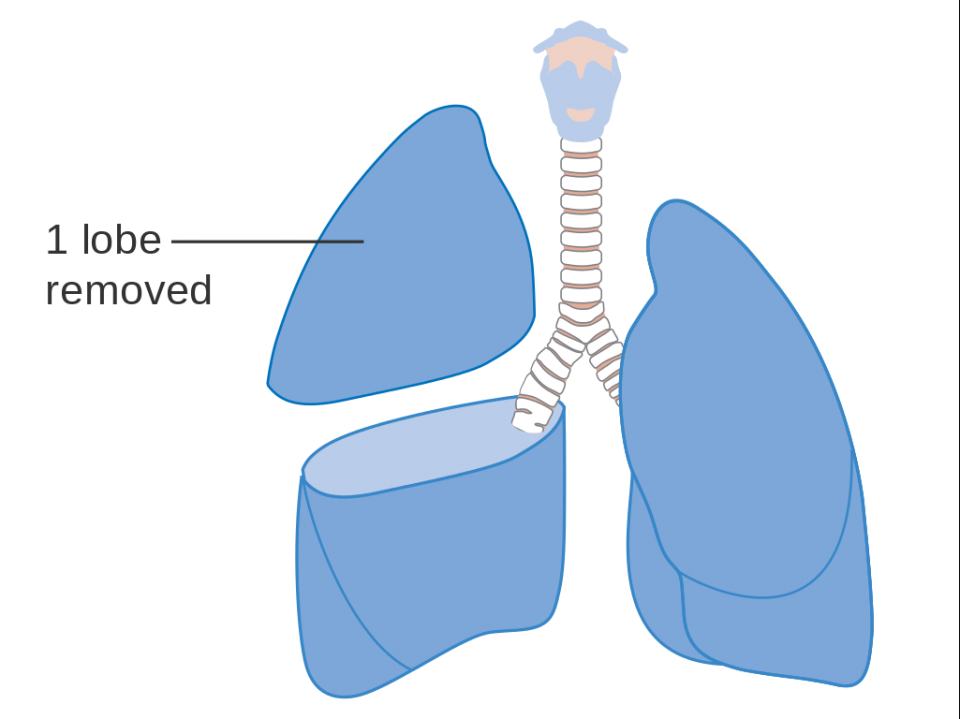
- Lobectomy: This is when a lobe of your lung is removed. Removal of 2 lobes is called bi-lobectomy. (Picture courtesy of CRUK / Wikimedia Commons)
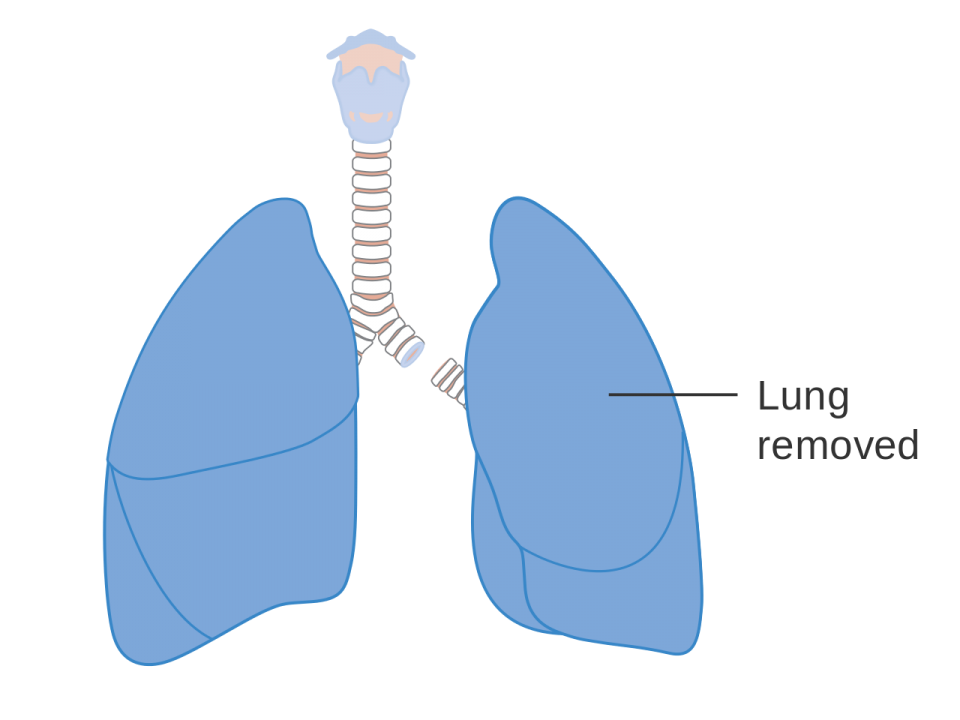
- Pneumonectomy: Here an entire lung is removed. (Picture courtesy of CRUK / Wikimedia Commons)
Sleeve resection: This is more technically challenging and involves removing the part of the lung with the cancer in it while preserving the remaining part of the lung, by reconstructing the airway and / or pulmonary arteries – it’s termed a parenchymal sparing resection. It is a preferred option to a pneumonectomy if possible and is the treatment of choice in high-volume cancer centres.
Lymphadenectomy (removal of the lymph nodes): During your surgery, the surgeon should remove a minimum number of the lymph nodes that are located close to and within the lung. This is in case they contain cancer cells that may have spread from the lung tissue. The minimum number of lymph nodes to be removed can vary. It depends on where the tumour is.
Wedge or sub-lobar resection: A section of a lobe of your lung is removed. This operation is only suitable when the cancer is less than 2cm in size and it is found on the periphery (edge) of the lung, with no evidence of cancer within any of the lymph nodes in the lung or chest. You should also have specific lymph nodes removed to assess and ensure accurate staging.
Segmentectomy resection: Removes slightly more of the lung than a wedge resection, in a way that follows the blood and airway supply of that segment or part of the lung. It is also very important that an appropriate number and location of lymph nodes are removed to ensure accurate staging.
During surgery, your surgeon will usually remove lymph nodes near the tumour and check them for cancer. Knowing if the cancer has spread to the lymph nodes helps your doctors decide if you need any other treatment.
Before surgery
You may have an assessment at a pre-admission clinic (PAC). You will have tests like a heart test (ECG) and lung tests.
Smoking and lung cancer surgery
If you are a smoker, it is important that you try to stop smoking at least 4 weeks before your surgery. Not smoking reduces your risk of developing complications after surgery.
Before your surgery you should meet your surgeon, anaesthetist and nurse specialist. They will discuss your surgery with you and you will have to sign a consent form. It is important to discuss with them if you do not understand anything or you have any questions or concerns. Read some general advice about getting ready for surgery.
Having surgery
There are 2 main ways of doing surgery for lung cancer:
- Keyhole surgery: The cancer is removed through 2-4 small cuts between the ribs, guided by a tiny camera. People often recover more quickly from keyhole surgery than from open surgery and the scars are smaller. Video-assisted and robotic-assisted thoracoscopic surgery (VATS and RATS) are types of keyhole surgery used for lung cancer. They are not suitable for every patient.
- Open surgery: The surgeon will make a cut (incision) in your chest to open it up by spreading the ribs so that he or she can do the operation to remove the cancer. You will have a larger scar afterwards. Open surgery is generally done for more advanced or technically complex cancer surgery.
Testing lymph nodes
Lymph nodes near the cancer will be removed during surgery. They will be checked for cancer cells. Knowing if the cancer has spread to the lymph nodes helps your doctors decide if you need any other treatment.
After surgery
Depending on the type of surgery you have had, you may be in a high dependency unit (HDU) for a few days after surgery.
You will have a few drips and drains in place - such as a chest drain, a drip with fluids and a catheter. It is normal to have these in place after an operation like this. You will be encouraged to sit out of bed and get moving around with the help of the nurses and physiotherapists.
As the days go on, you should begin to feel better and stronger in yourself and these drips and drains will be removed.
Read some general information and advice about what to expect after surgery.
Going home
Most people are ready to go home 1-2 days after robotic surgery and 5-7 days after open surgery. Before you go home you will have a chest X-ray to make sure your lung is working properly.
Your nurse will check your wound to make sure it is healing and talk to you about signs of infection to look out for when you are home.
If you live alone or have problems getting around the house, speak with your nurse. They will be able to help organise any community services you need after you leave the hospital.
Shortness of breath after lung cancer surgery
Some patients may feel short of breath because they have less lung tissue to supply their body with oxygen. Usually, this gets better as your body adapts and heals after surgery.
A physiotherapist will show you how to cough and turn in bed. The physiotherapist will also show you how to do breathing exercises and use equipment such as an incentive spirometer or an exercise bike. By doing the exercises, you will help to re-expand the remaining lung tissue, increase your lung capacity and get rid of excess fluid and air in your lung.
Incentive spirometer
An incentive spirometer is a device that tries to exercise your lungs and improve your breathing. When you breathe in with your mouth over a mouthpiece it makes a ball in a tube rise up. The physiotherapist will ask you to try to keep the ball up at the top of the tube for a few seconds by holding your breath. Gradually you can change the settings on the device to increase the level of exercise.
For more information
Phone
1800 200 700



