Having a risk factor doesn’t mean you will get cancer. Sometimes people with no risk factors get the disease.
Uterine (womb) cancer
About 570 women are diagnosed with uterine cancer every year in Ireland. Most uterine cancers occur in women aged 50 to 64.*
Signs and symptoms
Learn about the signs and symptoms of uterine (womb) cancer. You are more likely to survive cancer if you find it at an earlier stage.
Treatment
There are a number of different treatments available for uterine (womb) cancer. Your medical team will explain the best treatment options for you.
What is uterine (womb) cancer?
Uterine (womb) cancer is when the cells in the uterus (womb) change and grow in an abnormal way. A group of these cancer cells can form a tumour.
Most women with uterine cancer will have a type called endometrial cancer. This is cancer that starts in the lining of the uterus (endometrium).
What is the uterus (womb) and what does it do?
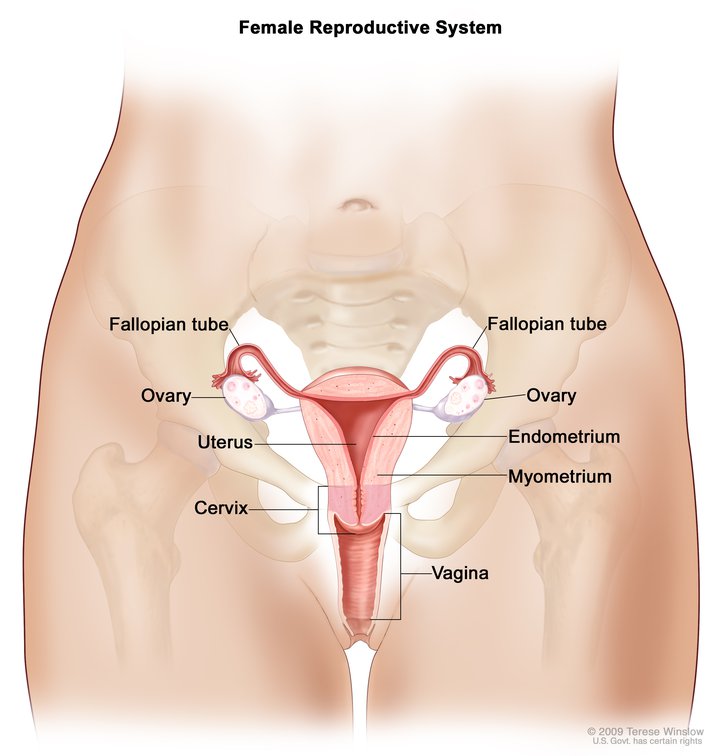
The uterus (womb) is a muscular, pear-shaped organ found in your lower abdomen, between your bladder and back passage (rectum).
It is part of the female reproductive system, together with the ovaries, the fallopian tubes, the cervix and the vagina. Uterus is the medical term for the womb.
The lining of your uterus is called the endometrium. Every month this lining thickens, grows and then falls away from the uterus as a monthly period. During pregnancy, your uterus protects the growing baby.
There are also layers of muscle in the uterus called the myometrium.
The lower part of the uterus is the cervix, which is also known as 'the neck of the womb'.
Although the cervix is part of the uterus, cancer of the cervix is diagnosed and treated differently to uterine cancer.
What are the types of uterine (womb) cancer?
There are two main types of uterine (womb) cancer:
- Endometrial cancer
- Sarcoma of the womb
Endometrial cancer: Nearly all uterine cancers (95%) affect the endometrium – the lining of the uterus. They are called endometrial cancers. The most common type of endometrial cancer is adenocarcinoma. Other less common types of endometrial cancers include:
- Clear cell carcinoma
- Serous carcinoma
- Carcinosarcoma – also referred to as MMMT. This is a mix of carcinoma and sarcoma
Sarcoma of the womb: This cancer affects the muscle layers of the uterus rather than the lining. The most common type is leiomyosarcoma. It is much less common than endometrial cancer.
Your doctor or specialist nurse will explain the type of uterine cancer that you have. The different types of uterine cancers can behave differently.
Knowing the type of uterine (womb) cancer you have will help your medical team to decide on the best treatment for you.
What increases my risk of uterine (womb) cancer?
The cause of uterine (womb) cancer is unknown. But there are risk factors that can increase your chance of developing the disease. These include:
It is more common in women after the menopause, between the ages of 50 and 64.
If you are overweight or obese, your risk of uterine cancer is increased.
If you are taking oestrogen-only HRT for a long time after the menopause, your risk of uterine cancer is slightly increased.
Family history of uterine cancer in a first degree relative (mother, sister, daughter). If you have an inherited faulty gene, it raises your risk of developing uterine or bowel cancer. In a small number of families, this faulty gene can cause a condition called Lynch Syndrome, which is also known as hereditary nonpolyposis colorectal cancer (HNPCC).
If you have not had children or never been pregnant, your risk of uterine cancer is increased.
If you have polycystic ovaries, your risk is increased. This is a condition where cysts grow in the ovaries.
If you started your periods early in life and/or started your menopause later, your risk is higher.
Taking tamoxifen for breast cancer can slightly increase your risk of uterine cancer. However, the benefit of taking tamoxifen for your breast cancer overrides the small risk associated with cancer of the uterus. But it is important if you are taking tamoxifen to tell your doctor if you have any unexpected vaginal bleeding or bleeding after your periods have stopped.
Note: We use gender-inclusive language. We sometimes use man/woman and male/female when they are needed to explain a person’s treatment and care – for example, talking about hormones or body parts – and when needed to describe research or statistics
Medical content updated from our 'Understanding uterine (womb) cancer' booklet (2023). Reviewed by Dr Razia Aslam, Consultant Gynaecological Oncologist, Sarah Mahony, Gynaecological Clinical Nurse Specialist and Linda Wilson, Daffodil Centre Nurse.
Continue reading about uterine (womb) cancer
For more information on uterine (womb) cancer, you can also look at This is GO, which gives tailored information for people worried about uterine cancer, people diagnosed with uterine cancer and for friends and relatives. This is GO is part of the Women's Health Initiative, a research project supported by the Irish Cancer Society.
Talk to a Cancer Nurse

Support Line
Our Daffodil Centres

*The Irish Cancer Society uses the most up-to-date cancer statistics from the National Cancer Registry Ireland, available on www.ncri.ie