What is the Gleason score?
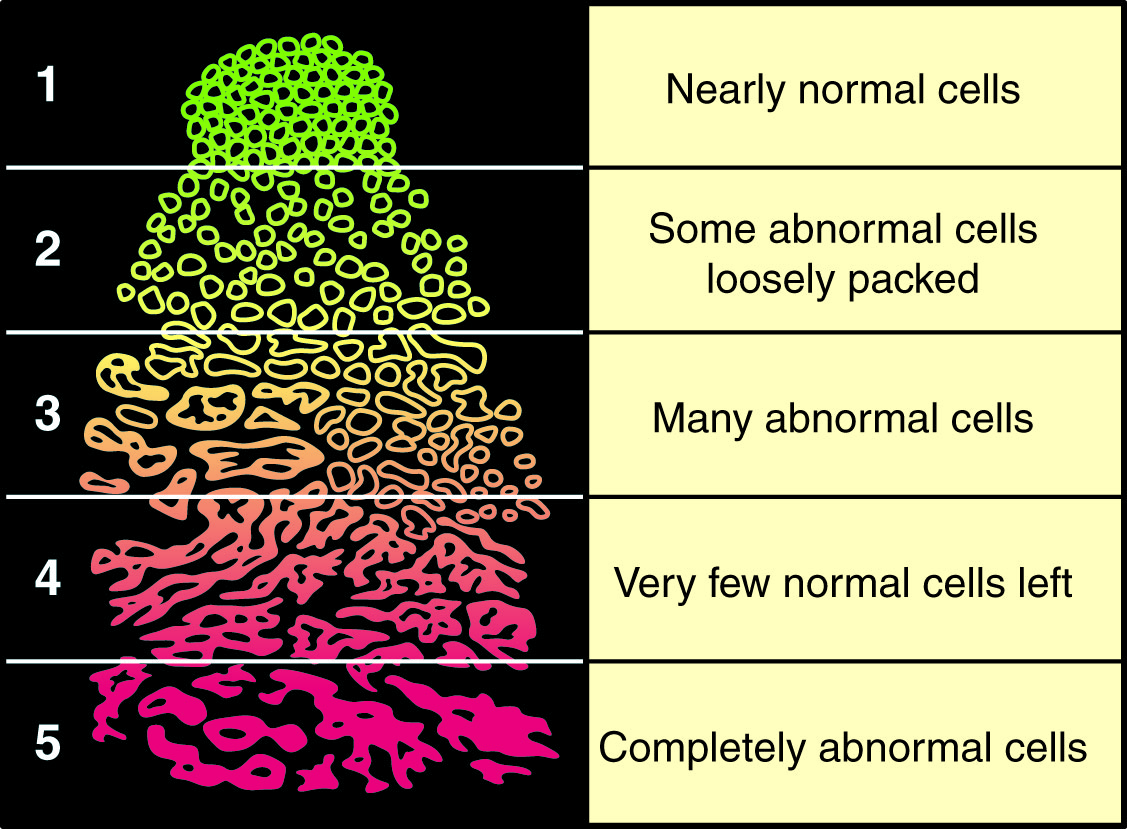
The Gleason score is a system used to describe the grade of prostate cancer.
If the most common grade in the sample is 3, and the second most common grade in the sample is 4, then your Gleason score will be 7 (3+4).
If only one grade is found, then this grade is added to itself. So if all the sample is only grade 3, then the Gleason score will be 6 (3+3).
- Lower grades are slower growing
- Higher grades are faster growing