Lung cancer
Lung cancer is the 4th most common cancer in Ireland, with almost 2,600* people being diagnosed each year. It usually affects people over the age of 50.
Signs and symptoms
Learn about the signs and symptoms of lung cancer. You are more likely to survive cancer if you find it at an earlier stage.
Treatments
There are a number of different treatments available for lung cancer. Your medical team will explain the best treatment options for you.
What is lung cancer?
Lung cancer is when normal cells in your lung grow in an abnormal way to form a lump called a tumour. Cells from this tumour may spread to other parts of the body.
Almost 2,600 people are diagnosed with lung cancer each year in Ireland.*
What is secondary lung cancer (lung metastasis)?
Sometimes cancer spreads to the lungs from somewhere else in your body, for example, from the breast or bowel. This is treated differently to cancer that starts in the lung (primary lung cancer).
If you want to know about another cancer type that has spread to the lung (metastatic cancer), please see our metastatic cancer page, speak to our cancer nurses on Freephone 1800 200 700 or visit a Daffodil Centre.
A short video about lung cancer, the signs and symptoms, types and treatments, and how to reduce your risk.
What are the types of lung cancer?
Most lung cancers are this type.
There are 4 main types of NSCLC:
- Adenocarcinoma: This is the most common type of lung cancer and is often found in the mucous glands that line the airways.
- Squamous cell carcinoma: This type of cancer is found in squamous cells, which are flat cells that line the inside of the airways in your lungs.
- Large cell carcinoma: This cancer may appear in any part of your lung. The cells are large and round when viewed under the microscope.
- Not otherwise specified (NOS): This is when the doctors cannot be sure which type of non-small cell lung cancer it is.
Genetic alterations (mutations) in NSCLCs
Some NSCLC cancers have genetic changes (mutations), which are not inherited. When these mutations occur in cells in the lungs, they affect the normal activity of the gene, and lung cancer can develop. Mutations in the EGFR, KRAS, ROS1 and ALK genes can happen in lung cancers – particularly in adenocarcinomas and in patients who have had little or no exposure to smoking.
About 1 in 7 of all lung cancers is the small cell type.
Small cell lung cancer begins in cells around the bronchi (airways) called neuroendocrine cells (NETs). SCLC cells appear small and round when looked at under a microscope and tend to grow quickly.
SCLC is an aggressive cancer with the potential to grow and spread rapidly. It often spread to lymph nodes and other areas such as your bones, brain, adrenal glands and liver.
This rare cancer affects the protective linings that cover your lungs. Usually it happens when someone is exposed to a chemical called asbestos.
Read more about mesothelioma
What are the lungs and what do they do?
The lungs are sponge-like organs in your chest. They allow our bodies to use oxygen by breathing. Your right lung is slightly bigger than your left and has 3 areas called lobes. Your left lung has 2 lobes. The area between the 2 lungs is called the mediastinum. It holds the heart, the oesophagus (food pipe), the trachea (windpipe) and many lymph nodes.
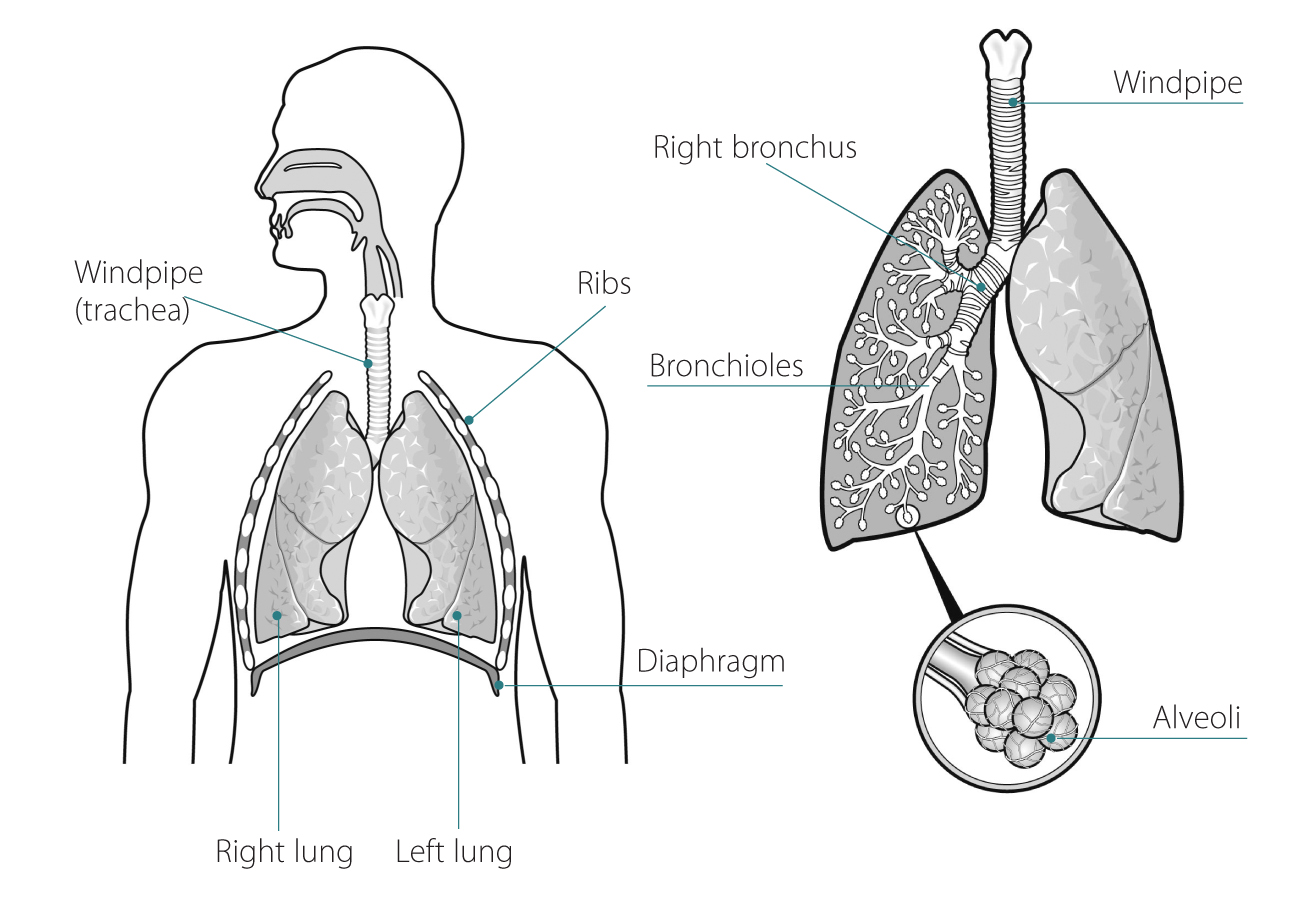
When you breathe in, your bring air into your lungs. Air passes from your nose or mouth through your trachea (windpipe).
From there it divides into 2 airways: the right and left bronchus, which each connect to a lung. The bronchi divide into smaller tubes called bronchioles. Air passes through these bronchioles and into tiny air sacs called alveoli.
The alveoli allow oxygen from the air to pass into your bloodstream when you breathe in. The bloodstream carries oxygen to the cells in your body. The cells need oxygen to live and carry out everyday functions. Carbon dioxide is a waste gas made during cell activity, and your body must get rid of it. Carbon dioxide moves from your bloodstream into the alveoli and leaves your body when you breathe out.
What increases my risk of lung cancer?
Smoking causes about 9 in every 10 lung cancers. The longer you have smoked, and the greater the number of cigarettes you have smoked, the greater the risk. Low-tar cigarettes do not reduce your risk. Those who smoke pipes and cigars have a lower risk of lung cancer than cigarette smokers, but they are at a much greater risk than non-smokers.
While smoking is the cause of most lung cancers, it is possible to get lung cancer even if you have never smoked. Anyone with lungs can get lung cancer. Other risk factors include:
Breathing in other people’s smoke also increases your risk of lung disease and cancer. But the risk is still much less than if you smoke yourself.
Certain chemicals such as asbestos, uranium, metal dust and fumes, nickel, paints, diesel exhaust, nitrogen oxides. These risks are higher if you smoke as well.
May be a risk where it is particularly bad.
Radon is a radioactive gas found naturally in the soil. But if your home traps it inside, it can build up and cause harm. Being exposed to radon gas in areas where levels are high can increase your risk of lung cancer. You can check the level of radon in your area on the [Environmental Protection Agency website].
If you have a parent, brother, sister or child who has had cancer which started in their lung, your risk is increased.
Having a risk factor doesn’t mean you will definitely get cancer. Sometimes people with no risk factors get the disease. If you’re worried, talk to your GP or talk to one of our cancer nurses. Call the Support Line on 1800 200 700 or visit a Daffodil Centre.
Reducing your risk of lung cancer
The most important thing you can do to reduce your risk of lung cancer is to stop smoking.
Medical content updated from our 'Understanding lung cancer and mesothelioma' booklet (2024), reviewed by Mr Gerald Fitzmaurice, Consultant Cardiothoracic Surgeon; Cr Claudia Carvajal Sanjines, Consultant Radiation Oncologist; Christopher Cronin, Specialist Registrar Medical Oncology; Clara Cremin, Clinical Specialist Radiation Therapist; Aine Ward, Cardiothoracic ANP; Anne Quinlan, Daffodil Centre Nurse.
Publications about lung cancer
Talk to a Cancer Nurse

Support Line
Our Daffodil Centres

*The Irish Cancer Society uses the most up-to-date cancer statistics from the National Cancer Registry Ireland, available on www.ncri.ie