Lung cancer
Diagnosis and tests
Diagnosing lung cancer
Your family doctor (GP) will talk to you about your symptoms. Your GP may organise for you to have a chest X ray, to check your lungs for any abnormal changes.
If your doctor thinks you need more tests, he or she will refer you to a rapid access lung clinic. These are consultant-led assessment and diagnostic services for patients with suspected lung disease. There are eight rapid access clinics located around the country. Your GP will send you to your nearest one. Tests you might have include:
Specialist technicians and doctors look at your sample under a microscope. They can identify and count different types of blood cells. Note, there is no blood test to diagnose lung cancer.
These are breathing tests. You blow into a mouthpiece to check how well your lungs work.
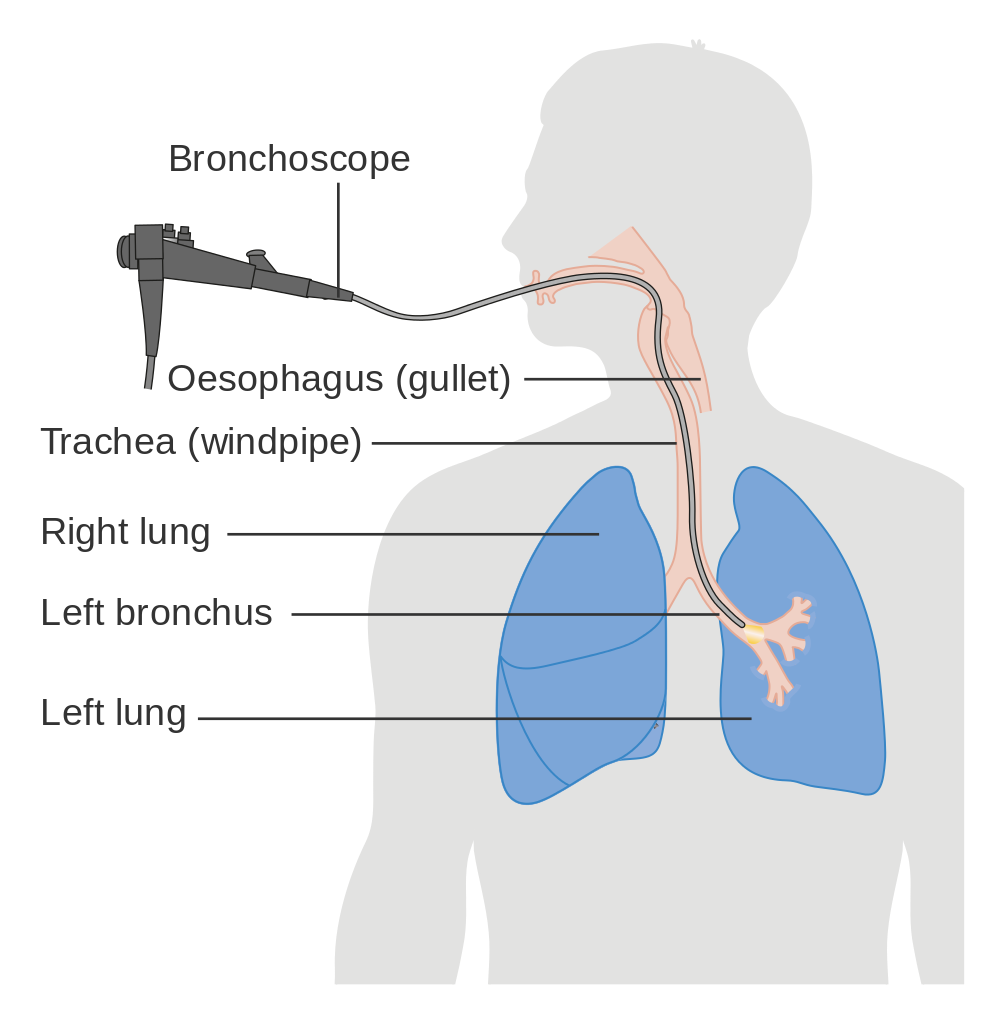
This test uses a long tube with a camera at one end to view the airways in your lung. A biopsy may be taken at the same time.
Read more about bronchoscopy.
A type of bronchoscopy that uses an ultrasound probe to look at the lungs and surrounding lymph nodes. Biopsy (tissue) samples from the lung or lymph nodes can be taken by passing a needle through the tube. This is called a transbronchial needle aspiration (TBNA).
Read more about EBUS.
During a bronchoscopy, EBUS or CT scan, your doctor can take small amounts of tissue samples from your lung. These are called biopsies. Biopsies are sent to a laboratory and looked at under a microscope. These biopsies will be examined to see if there are any gene mutations or proteins on the cancer that specific treatments can target.
Results of all these tests are usually available within a month. The clinic will contact you to come back to the clinic for your results.
A respiratory doctor is a doctor who specialises in treating problems with the lungs and respiratory (breathing) system.

If you are diagnosed with lung cancer, we're here for you.
Our cancer nurses are here if you need information or just want to talk. They can help you to understand your diagnosis and what to expect, send you information and tell you about our services.
Further tests for lung cancer
The tests you have will give your doctors more information about your general health and about the cancer. The tests will help to stage your cancer. This means finding out
- How large is the cancer?
- Where exactly is the cancer?
- Has the cancer spread to any other parts of your body?
Some tests may also be used to see how well your lungs are working and how you are responding to treatment.
Tests you may have include:
Blood tests can help to check your general health. They will be done regularly during your treatment.
A type of X-ray that gives a detailed picture of the tissues inside your body.
Sometimes, a small sample of tissue is taken from your lungs in a test called a CT-guided lung biopsy. The sample is taken using a thin needle and sent to a laboratory for analysis.
As well as a CT scan of your lungs, your doctor may do a CT scan of your abdomen/pelvis and/or brain.
A radioactive injection that will show up any cancer spread to other parts of your body on a CT scan picture.
A small tube with a camera on the end is passed into your lungs to take pictures of your lungs. Biopsies (tissue samples) can also be taken during the procedure. Biopsy samples can give information about your type of cancer and how fast it is growing.
A type of bronchoscopy that uses an ultrasound probe on the end of the brochoscope to take pictures of the lungs and surrounding lymph nodes. The pictures can show how big the tumour is and whether any nearby lymph nodes are enlarged. Biopsy (tissue) samples from the lung or lymph nodes can be taken by passing a needle through the tube. This is called a transbronchial needle aspiration (TBNA).
Similar to an EBUS, but the tube with the ultrasound probe goes down your oesophagus (gullet) to give images of the area around the heart and lungs, to show if any of the lymph nodes in the centre of the chest are enlarged.
A fine needle can be passed along the tube to take tissue samples from the lymph nodes.
Putting a tube with a light and a camera into the centre of your chest area, through a small cut in the front of your lower neck. It can see if there are any abnormal areas.
This is a test to look at the membranes that line the lungs (pleura).
A thoracoscope is a long tube with a camera. You will have a general anaesthetic for this operation. Your surgeon will make a cut between two ribs and put the thoracoscope in. This allows them to see if the pleura appear normal.
The surgeon can also take biopsies (tissue samples) of the lining of the inside of the chest and / or the lymph nodes. They can perform a pleurodesis (drain fluid from the lungs), if needed
A radioactive injection that can show areas of abnormal bone on a scan, which may be caused by cancer.
Your doctor will organise a range of breathing tests to check how well your lungs are working and to see what treatments are possible. The main type of breathing test is a pulmonary function test (PFT), which is where you blow into a mouthpiece on a machine. The test is not painful and takes about 20 minutes. Cardiopulmonary exercise testing (CPET) assesses how your lungs and heart respond to exercise, using an exercise bike.
A scan that uses magnetic energy to create a picture of the tissues inside your body. An MRI scan may need to be done to see if the cancer has spread beyond your lung.
MRI scans are not often used for lung cancer unless the cancer is very close to the top of the lung, or other tests suggest an MRI scan is needed.
The tests you have can help to:
- Stage your cancer. This means finding out the size and position of the cancer.
- Grade your cancer. Grading describes how quickly the cancer may grow and spread and how it might respond to treatment.
Some tests may be used see how you are responding to treatment.
Staging tests are important as they help your medical team decide on the best treatment for your cancer.
Waiting for test results
While some results may come back quickly, others may take a few weeks. Waiting for results can be an anxious time. It may help to talk things over with your doctor or nurse or with a relative or close friend. You can also call our Support Line on 1800 200 700 or visit a Daffodil Centre to speak to a cancer nurse.
Staging for non-small cell lung cancer
Staging means finding out how big the cancer is and if it has spread to other parts of your body. Staging will help your doctor to plan the best treatment for you.
TNM staging system
The staging system normally used is called TNM. This stands for:
This describes the tumour size and where it is located in the lungs.
• N0: No lymph nodes are affected.
• N1: Some lymph nodes near where the airways join the lungs are affected.
• N2: Some lymph nodes in the centre of the chest or where the trachea enters the lung are affected.
• N3: Some lymph nodes on the opposite side of your chest to where the tumour is, or near your collarbone, are affected.
• M0: The cancer has not spread to other parts of the body.
• M1: The cancer has spread to other parts of the body.
Number staging
Your doctor often uses the TNM information to give your cancer a number stage – from 1 to 4. A higher number means a more advanced cancer.
Stage 1
The cancer is inside the lung (localised) and has not spread to nearby lymph nodes.
Stage 2 and 3
The cancer may be larger and may affect the nearby lymph nodes or surrounding tissue.
Stage 4
The cancer has spread to a distant part of the body such as the liver, bones or the brain.
Knowing the stage of your cancer helps your team to plan the best treatment for you.
Staging for small cell lung cancer
More and more doctors are using the TNM and number staging system to stage small cell lung cancer. However, some will describe your cancer as a limited stage disease or extensive stage disease.
Limited stage: This usually means the cancer is in one lung.
Staging can be hard to understand, so ask your doctor and nurse for more information if you need it.
Continue reading about lung cancer




Get help & support

Support Line
Free support pack

