Melanoma
Signs and symptoms
Symptoms of melanoma
The most common symptoms of melanoma are:
- A mole that suddenly gets bigger or you find a new one on your skin
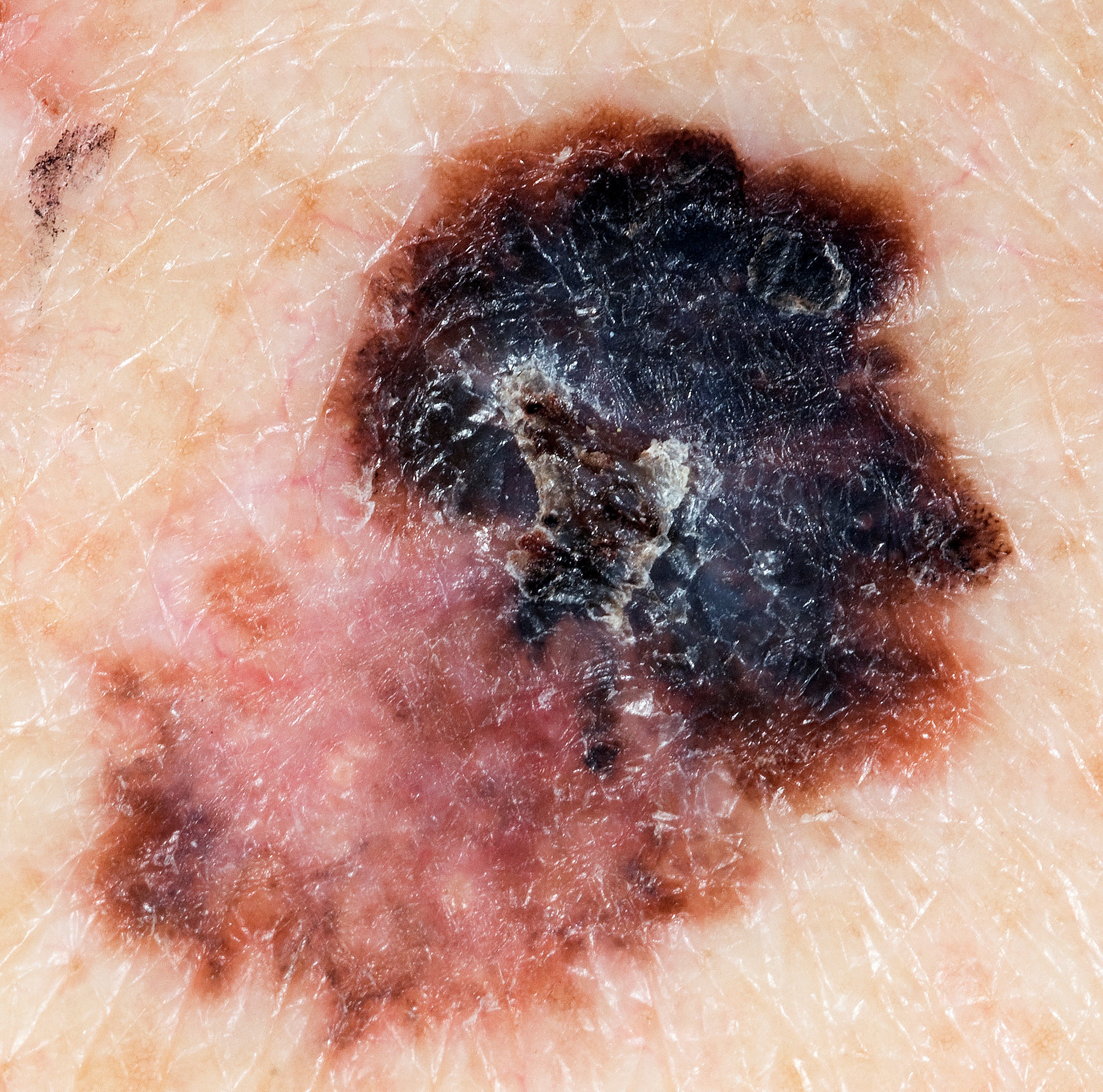
- A mole that develops a ragged or uneven outline
- A mole with a mixture of different shades of brown, black or other colours through it
- A mole that is bigger than the blunt end of a pencil
- A mole that looks red or inflamed around the edges
- A mole that is bleeding, oozing or crusting
- A mole that starts to feel different, for example, slightly itchy or painful
Skin changes aren’t necessarily cancer. But it’s important to go to the GP and get any unusual changes checked.
If melanoma is diagnosed and treated early there is a very good chance of a cure.
Checking moles
When checking a mole, look for the ABCDE
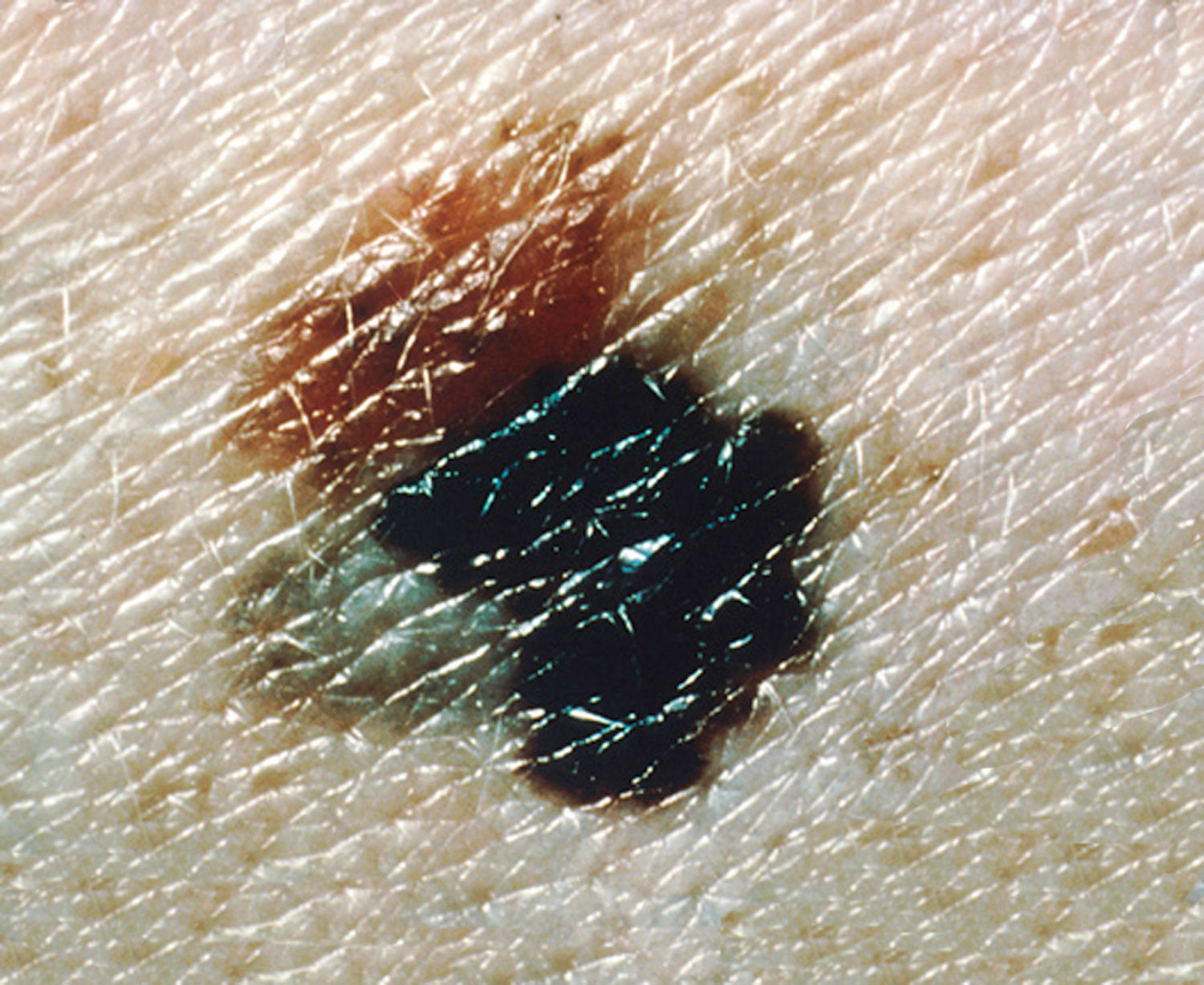
Asymmetrical moles
A change in shape - one half is unlike the other.
Border of a mole
A change in the edges: they look blurred or jagged.
Colour of a mole
A change in the colour or differences within the mole: shades of tan, brown, black or even white, red or blue.
Diameter (width)
Any change in size. Most melanomas are larger than 6mm (the size of the
top of a pencil) and keep growing.
Evolving
Melanoma moles often change (evolve).
Can I be screened for melanoma?
Testing for melanoma when you have no symptoms is called screening. There is no national melanoma screening programme in Ireland at present.
If you have a risk factor for melanoma, talk to your doctor about getting checked.
Spotting skin cancer early
The best way to check for early signs of melanoma is to check your skin for changes every month. This can help you to learn the moles, freckles and other skin marks that are normal for you.
Continue reading about melanoma
Talk to a Cancer Nurse

Support Line
Our Daffodil Centres