Ovarian cancer
Diagnosis and tests
Diagnosing ovarian cancer
Your family doctor (GP) will talk to you about your symptoms and may examine you by placing a gloved finger into your vagina to feel for any lumps or swelling.
Your GP will refer you to hospital if they think you need more tests. Tests you might have include:
A device like a microphone passed over your tummy to give a picture of the tissues inside your body. It can show any abnormal changes.
Read more about ultrasound scans.
A small probe is put into your vagina to produce clear pictures of your womb and ovaries.
Read more about ultrasound scans.
A thin flexible tube with a camera attached to it is passed through a small cut in your tummy. The lets your doctor look for any abnormal changes in your ovaries and take sample of cells (biopsy). The test is done under general anaesthetic. You will have some stitches in your tummy after the test.
Read more about having a laparoscopy.
CA125 is a chemical found in blood that is sometimes released from ovarian cancer cells. It is known as a tumour marker for ovarian cancer. Not all women with ovarian cancer will have a raised CA125.
A sample of the cells is taken and looked at under a microscope in the lab to see if there are any cancer cells. The biopsy can be done during a laparoscopy.
A gynaecologist is a doctor who specialises in treating problems with women’s reproductive systems, e.g. vagina, vulva, womb (uterus) and ovaries.

If you are diagnosed with ovarian cancer, we're here for you.
Our cancer nurses are here if you need information or just want to talk. They can help you to understand your diagnosis and what to expect, send you information and tell you about our services.
Further tests for ovarian cancer
You may need further tests to give your doctors more information about your general health and about the cancer. For example:
A scan that uses magnetic energy to build up a picture of the tissues inside your body. During the scan you will lie inside a tunnel-like machine.
Read more about MRI scans.
A type of X-ray that gives a detailed picture of the tissues inside your body.
Read more about CT scans.
A radioactive injection that will show up any cancer spread to other parts of your body on a CT scan picture.
This uses a tiny camera attached to a flexible tube, which is passed into your stomach through your mouth. It can check the lining of your stomach to see if there are any cancer cells there.
Blood tests may be done to check your general health and how well your liver and kidneys are working. A blood test called CA125 will also be done. This tests for a protein called CA125 in the blood. CA125 is known as a tumour marker for ovarian cancer, because it is sometimes released from ovarian cancer cells into the blood. Not everyone with ovarian cancer will have high levels of CA125 in their blood. But if there is a high level, it may give your doctor extra information to help them plan your treatment. It will also help your doctor to measure how well you are doing during or after treatment.
This test is carried out in the X-ray department of the hospital. Before the test you must empty your bladder. You will then be asked to lie on your back. A small metal device called a probe is put into your vagina. It looks like a microphone and gel is placed on it. By doing the test in this way clear pictures of your womb, fallopian tubes and ovaries can be built up using sound waves. This test may be uncomfortable but is not painful.
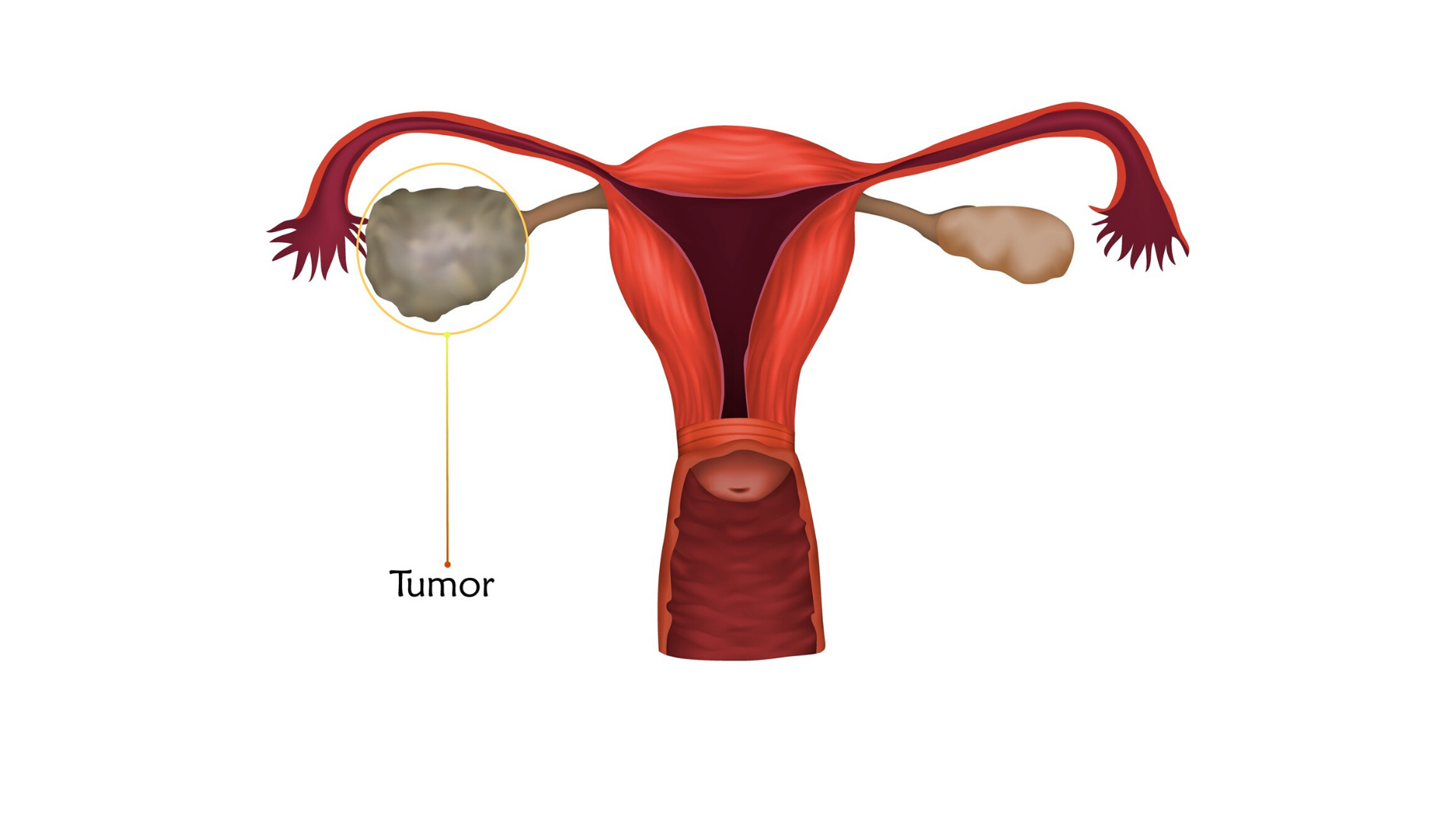
This involves taking a biopsy (tissue sample) from your ovaries and possibly from the omentum, a fatty pad of tissue inside your stomach. Image-guided means that the doctor will use an ultrasound or CT scan to guide the needle into the stomach to where the tumour is.
The doctor will use local anaesthetic to numb the area where the needle is inserted. You may also be given some sedation. The procedure can take between 10 and 20 minutes. You’ll need to stay in hospital for a couple of hours after the biopsy, and possibly overnight. This is because there is a risk of bleeding afterwards. If you’ve been given sedation, you’ll need someone to take you home and stay with you for 24 hours until the effects have completely worn off.
This test allows your doctor to look at your ovaries and nearby tissues. It can help the team confirm the stage of the cancer, plan surgery or other treatments and decide how best to manage your cancer. It is a small operation done in theatre under a general anaesthetic.
While you are asleep, your doctor makes a small cut in your lower abdomen, near your belly button. They then put a thin mini telescope called a laparoscope into the wound. By looking through the laparoscope your doctor can see your ovaries and take a small sample of tissue (biopsy) and have it examined.
If you get a build-up of fluid in your abdomen (ascites) a sample can be taken to see if it has any cancer cells. Your doctor will first numb an area of your abdomen before putting a small needle through your skin. This needle can be inserted with the help of ultrasound. Some fluid is taken and then examined under a microscope.
The tests you have can help to:
- Stage your cancer. This means finding out the size and position of the cancer.
- Grade your cancer. Grading describes how quickly the cancer may grow and spread and how it might respond to treatment.
Some tests may be used see how you are responding to treatment.
Waiting for test results
While some results may come back quickly, others may take a few weeks. Waiting for results can be an anxious time. It may help to talk things over with your doctor or nurse or with a relative or close friend. You can also call our Support Line on 1800 200 700 or visit a Daffodil Centre to speak to a cancer nurse.
What are the stages of ovarian cancer?
Staging means finding out how big the cancer is and if it has spread to other parts of your body. Staging will help your doctor to plan the best treatment for you. Sometimes your cancer will only be staged after surgery.
TNM staging system
The staging system normally used is called TNM. This stands for:
- Tumour (T) How big is the tumour?
- Node (N) Is there cancer in the lymph nodes?
- Metastasis (M) Has the cancer has spread?
Number staging
Your doctor often uses the TNM information to give your cancer a number stage – from 1 to 4. A higher number means a more advanced cancer.
Most ovarian cancers are diagnosed at stage 3 or 4. This is because with early-stage ovarian cancer there may be few or no symptoms.
Stage 1 cancer affects only your ovaries.
- 1a:The cancer is in one ovary only. The capsule around the ovary is
intact (not broken). - 1b: Like stage 1a except the cancer is in both ovaries.
- 1c: Tumour is in one ovary or in both ovaries, along with one of the
following:
- 1c1: The capsule around the ovary breaks (ruptures) during surgery. This is called surgical spill.
- 1c2: The capsule breaks before surgery OR there is cancer on the surface of 1 or both ovaries.
- 1c3: There are cancer cells in the fluid in your abdomen (ascites) OR There are cancer cells in the peritoneal washings. Peritoneal washings refers to liquid used to wash the area around the organs in your abdomen and pelvis during surgery. The liquid is checked for cancer cells.
Stage 2 cancer has spread outside your ovary / ovaries but is still within your pelvis.
- 2a: The cancer cells have spread to organs near your ovary, such as your womb or fallopian tubes.
- 2b: The cancer has spread to other organs in your pelvis, such as the lining of your lower bowel or bladder.
Stage 3 cancer has spread outside your pelvis and into your abdominal cavity. It can affect the lining of your abdomen or lymph nodes there. These are called retroperitoneal lymph nodes. When lymph nodes have cancer in them they are called positive lymph nodes.
- 3a1: The cancer has spread to the retroperitoneal lymph nodes.
- 3a2: Cancer cells affect the lining of your abdomen but they are very tiny and can only be seen under a microscope. May or may not
have positive retroperitoneal lymph nodes. - 3b: The cancer in your abdomen can be seen with the naked eye but is smaller than 2cm across. May or may not have positive
retroperitoneal lymph nodes. - 3c: The cancer in your abdomen can be seen with the naked eye and is larger than 2cm. May or may not have positive retroperitoneal
lymph nodes. May have spread to the capsule around the liver or spleen.
Stage 4 cancer has spread to other organs away from the pelvis.
- 4a: There are cancer cells in the fluid between the membranes that cover the lungs (pleural fluid).
- 4b: The cancer has spread to the inside of other organs such as the lungs, the liver, the spleen, the brain. Also includes when the
cancer has spread to lymph nodes outside the pelvis, such as the groin, the neck, the armpit or the chest.
Knowing the stage and grade of your cancer helps your team to plan the best treatment for you.
Recurrent ovarian cancer
What are the grades of ovarian cancer?
The grade of the cancer can help the doctor to predict how quickly the cancer will grow. You can have a low, moderate or high grade cancer. Lower grades are slower growing. Different grades may need different treatments.
The cancer cells are very like normal cells in your ovary. They usually grow slowly and are less likely to spread.
The cancer cells look less like normal ovarian cells.
The cancer cells are very unlike normal ovarian cells. They usually grow quicker and are more likely to spread.
Staging and grading can be hard to understand, so ask your doctor and nurse for more information if you need it.
Continue reading about ovarian cancer




Get help & support

Support Line
Free support pack

