Urostomy
Surgery for muscle-invasive bladder cancer
You may have surgery to remove all or part of your bladder (radical or partial cystectomy) if you have muscle-invasive bladder cancer.
Radical or total cystectomy
Surgery to remove your bladder is called a cystectomy.
- Partial cystectomy: The surgeon removes just part of your bladder.
- Radical or total cystectomy: The whole bladder is removed, along with nearby tissues, lymph modes and organs. For example, seminal vesicles, prostate and part of urethra (men and people assigned male at birth) and ovaries, womb, cervix, part of vagina and urethra (women and people assigned female at birth).
Having all or part of your bladder removed is major surgery. It is only carried out in a small number of hospitals (specialist centres). You may have to travel to your nearest specialist centre to talk to your surgeon about the operation and to have the surgery done.
The type of procedure you have will depend on the stage of the cancer and your general health.
What are the ways of doing surgery?
Your bladder can be removed with open surgery or keyhole surgery. Discuss your preference and your options with your surgeon.
Most cystectomies are open surgeries.The surgeon makes a single cut in your lower abdomen (tummy area).
A few small cuts are made in your abdomen. A tube with a light and camera and special instruments are put in through the cuts. The urologist uses a
computer and robotic arms to help to remove your bladder.
Ways of draining urine after cystectomy
If your whole bladder has been removed, your surgeon will need to find a new way to drain your urine. This is done at the same time as the cystectomy.
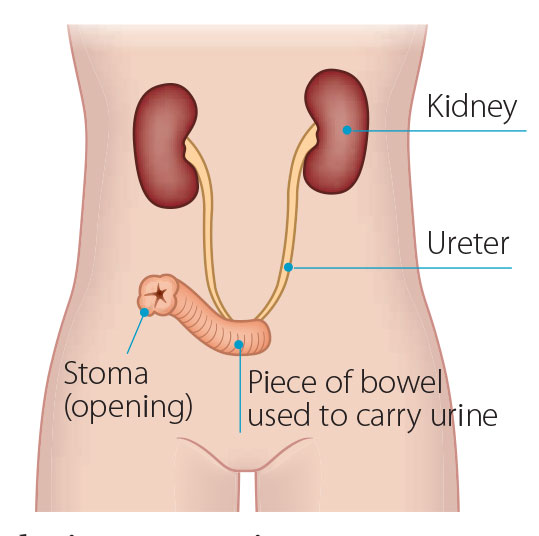
Your surgeon will use part of your small bowel to bring urine to an opening outside your body. This is known as a urostomy or an ileal conduit.
Your surgeon uses about 6 inches (15cm) of your small bowel to make a tunnel. The 2 kidney tubes (ureters) will then be attached to it.
One end of the passage is closed up with stitches, while the other end is brought through to the surface of your tummy. The open end is called a stoma and looks like the skin inside your cheek. You will need to wear a bag attached to the stoma to collect and drain your urine.
A flat, watertight bag is placed over the stoma to collect your urine. The side of the bag that is placed on the skin around the stoma has a paste that seals onto the skin. The bag will fill with urine and you will need to empty it regularly. A stoma nurse will show you how to take care of it.
With this type of urinary diversion, you don’t need an external bag to collect your urine.
Your surgeon uses a piece of your bowel to make an internal pouch that can store urine inside your tummy. The 2 kidney tubes (ureters) will then be attached to it. Urine will drain through the ureters into this pouch. The internal pouch that replaces your bladder is connected to your tummy wall by a stoma (opening).
Your surgeon will create a one-way valve to keep the urine inside the pouch. You empty urine from the pouch through the stoma using a thin tube called a catheter. You will need to do it about 5 or 6 times a day. A stoma nurse
will teach you how to do it. In this case, you do not need a urinary pad or bag.
The stoma opening is covered with a bandage.
The surgeon makes a pouch out of bowel tissue. The kidneys drain the urine into this pouch. The pouch is then connected to your urethra. The pouch (known as a neobladder) stores urine like your bladder did, and you pass urine out through your urethra.
You can empty the pouch by holding your breath and pushing down into your tummy. You will need to do this regularly as you won't know when your bladder is full. Your hospital team will give you more information about this.
Possible side-effects of bladder surgery
With all surgeries there is a small risk of bleeding and infection. For example, infection in your wound, chest or urine. Your doctors and nurses will watch you closely to make sure these risks are reduced, or treated quickly if they happen. You can also help to prevent infection yourself by having good hygiene and doing deep-breathing exercises.
There is a risk of blood clots in the lungs or legs. Doing the breathing and leg exercises the physiotherapist gives you after surgery can reduce this risk.
There is a risk of urine leakage from the newly formed pouch in the first few days after surgery.
There is a small risk that your bowel will become inactive and take a while to return to normal. This is known as paralytic ileus. It can happen after any surgery that involves handling of the bowel. There is also a very small risk of a bowel leak. This is because your bowel has been divided to take a part out and the two ends have been joined together.
Surgery to remove your bladder can damage the muscles and nerves in the pelvic area, which can cause physical problems when having sex. It may make sex more uncomfortable or you may have a loss of libido (sex drive).
Sex may feel different and your orgasms may be affected. There are also emotional issues relating to a change in body image and loss of libido (sex drive).
Shortening or narrowing of the vagina: Bladder surgery or radiotherapy might shorten or narrow your vagina. This can make sex uncomfortable. Regular gentle sex or using a special device called a dilator can help with this side-effect. Dilators are tampon-shaped plastic tubes of different sizes that you use with a lubricant. Your specialist nurse will advise you on how helpful a dilator may be in your situation and explain how to use them. You may feel embarrassed or uncomfortable, but your specialist nurse will understand your concerns and will always respect your feelings.- Erectile dysfunction: You may find it hard to get or keep an erection after surgery or radiotherapy for bladder cancer. This is called erectile dysfunction or impotence. There are medications and other treatments that can help with erectile dysfunction. For example, tablets, injections, vacuum pumps or implants to help you get an erection. Your doctor can advise you about treatment that may help. After a cystectomy you will be unable to father a child naturally.
Caring for a urostomy
After urostomy surgery, your urine will pass down the ureters from your kidneys, through the piece of bowel and out through the stoma (opening)
You will need to wear a waterproof bag over the stoma to collect the urine. This bag is called a urostomy bag and it sticks to the skin around the stoma. You can empty the bag as often as needed.
For the first 7 to 10 days, fine plastic tubes will be placed up through the ureters. These are called ureteric stents and they support the new system while healing occurs. The stents can be seen coming out of the stoma into the urostomy bag. They will usually be removed by your stoma nurse before you go home.
It can take a while to adjust to having a stoma. Your stoma nurse and other nurses will teach you how to care for your urostomy. They will show you how to put the bag on correctly so that it protects the skin around the stoma from the urine, which could make your skin sore.
Tips for managing a urostomy / stoma
- The stoma bag will usually last 3 to 5 days. Do not change it earlier unless needed. If you remove the adhesive flange more frequently, it may irritate and damage the skin around your stoma, causing soreness.
- If the stoma bag leaks, change it as soon as you can.The longer your skin is exposed to urine, the more your skin might suffer.
- The stoma bag will not stick so well to moist or damaged skin. This may cause odours and leaking bags.
- Empty the stoma bag before it gets too full as the weight of the urine may ‘pull’ on the flange. This can cause the flange to come away from your skin.
- It is normal to find mucus in your urine. The part of your bowel used to form the urostomy makes the mucus.
- Make sure you are using a stoma bag of the correct size. Your stoma may get smaller as time goes by.
When you leave hospital, you will be given some dressings and urostomy bags to last a few days. You will also be given a prescription for more supplies from your stoma nurse. Go to the pharmacy to get these as soon as possible. Most pharmacies do not keep them in stock and it may take a few days for supplies to arrive. Some pharmacies have a direct delivery service where you can
telephone in your order and they will send out your supplies by post. Ask your stoma nurse if this service is available in your area.
Keep enough supplies so you don’t run out. You may wish to keep a spare stoma bag in the car or at work in case the stoma bag needs to be changed. Keep a plastic bag handy for getting rid of used supplies.
It can take a while before you feel confident about managing the urostomy bags. The community stoma nurse can visit you at home to discuss any
concerns. You may also find it helpful to talk to someone who has learned to live with a urostomy. Your nurse may be able to arrange for someone to talk to you and tell you about how they coped. This advice can be very helpful, especially in the first few months after your operation.
There are many stoma accessories to help make life more comfortable. These include girdles, support belts, deodorisers, wipes, skin protective wipes, lotions and creams, adhesive removers, stoma paste, rings and disposal bags. There are also snug clothes like underwear and swimwear you can wear. Talk to your stoma nurse about what is best for you.
Having a urostomy can affect how you feel about your body. You may also be afraid that the urostomy bag will become dislodged or cause damage to the
stoma. Empty the bag before sexual intimacy and roll it up or tape it down so it will not get in the way, if you wish. If you need more advice talk to your doctor, specialist nurse or stoma nurse, they are all experienced in dealing with these issues.
When you go on holiday, remember to take enough supplies with you. Keep your supplies in your hand luggage in case your suitcase gets lost. Travel certificates are available from your stoma nurse to help you bring your supplies through security at the airport.
Stoma support and advice
- Your stoma nurse and other nurses will teach you how to care for your urostomy at hospital.
- The community stoma nurse can help you once you go home.
- Someone who has already learned to live with a urostomy may have useful tips on managing the bag. Ask your nurse if they can put you in touch with someone.
Talk to a Cancer Nurse

Support Line
Our Daffodil Centres