Treating children's cancer
If your child has been diagnosed with cancer we have information about how children’s cancers are treated including treatment types, side-effects and medical language.
Getting ready for treatment
Preparing your child for treatment
It’s best to be as honest as you can about what will happen. Young children only need simple explanations and older children might need more detail. Children may be curious about how a hospital ‘works’. It may be possible for a member of staff to explain how different pieces of equipment work.
Your child may like to take part in the Beads of Courage programme. For every kind of test or treatment they have, they receive a coloured bead. They can collect these beads to keep track of their cancer journey and show how brave they are.
You will be asked to sign a consent form saying that you understand what the treatment is for and that you give permission for treatment to be given.
Before treatment, you should be fully informed about:
- What the treatment is for
- The type and amount of treatment your child will have
- The benefits and risks of the treatment
- Possible side-effects from treatment
- Any other treatments that may be available
If you are confused about the information or if you have any worries about the treatment let your doctor or nurse know straight away. Once a child reaches the age of 16, they can usually consent to their own treatment.
Many children are fitted with a central line. This is a tube that goes directly into a vein and stays in place throughout treatment. Any treatment or medication that needs to go into their veins can be delivered through the line, and blood can be taken from it. This means your child won’t need repeated injections. A Hickman or Freddie line is a type of central line. It is inserted into a large blood vessel in your child’s chest under general anaesthetic. We have more information on children’s central lines and advice on caring for them.
Your child may have more tests and procedures before treatment starts. For example, tests to check their general health before surgery or radiotherapy planning sessions, if they are having radiotherapy.
Treatment types
Chemotherapy uses anti-cancer drugs to kills cancer cells. Your child may have one drug or several, depending on their protocol (treatment plan).
Radiotherapy is a painless treatment using high-energy X-rays that go deep inside the body to kill cancer cells.
Targeted drug therapies target certain parts of cancer cells.
Immunotherapy treatment helps your immune system to work better to fight cancer cells.
Stem cell transplant replaces diseased or damaged blood cells with cancer-free stem cells.
Surgery involves making a cut in your child's body to remove tissue or to insert a central line for treatment.
Your child may need surgery for various reasons, for example:
- Diagnostic tests. For example, a lumbar puncture, bone marrow or other biopsy.
- To have a Hickman catheter or port put in for treatment.
- To have a tumour removed.
A clinical trial is a study of a treatment. Cancer clinical trials are done to find new and better treatments for cancer. Some studies look at new drugs; others look at drugs that have been used for a long time to see how well these drugs work in different combinations. Trials can also look at other forms of treatment, such as surgery or radiotherapy, or quality of life.
Children in Ireland most often take part in trials that compare a new drug or combination of drugs against the standard treatment at the time to see which works best. Patients may be picked by chance by a computer in the trial centre (randomly) to receive either standard treatment or the new treatment. This is called randomisation and may happen at different points along the treatment protocol.
Palliative care is the phase of treatment where cure is no longer possible. Palliative care describes the supportive care and treatment given to ease symptoms and improve quality of life, but with the knowledge that it will not lead to a cure.
Supportive care medications are medicines that are used to help with side-effects of treatment. They do not cure or treat cancer. You may need to give your child these medicines at home. Common supportive care medicines are:
- Anti-sickness medicines (anti-emetics)
- Pain relief
- Laxatives (to help your child poo if they have constipation)
- Antibiotics to prevent infection (prophylactic antibiotics)
- GCSF – Injections to help the white blood cell count recover.
If the medicine isn’t helping with the problem, for example, if your child is still vomiting or in pain, contact the hospital.
The medical words your doctors and nurses use may seem like a foreign language. It can be frustrating or upsetting if you don’t understand the information you’re given about your child’s illness or treatment.
It’s important to understand your child’s cancer, treatment and side-effects and to get help with any problems you’re having. Don’t be left with unanswered questions or worries - our tips and glossary of medical language can help you.
Will my child get side-effects?
Side-effects include being more at risk of infections, feeling sick and hair loss. Most side-effects get better in the weeks and months after treatment. Some treatments can cause long-term side-effects such as damage to organs or infertility.
The side-effects your child might get depend on the type of treatment, the dose, how long they have treatment for and their general health.
Your doctor or nurse will discuss any possible side-effects with you before treatment. Read about the different treatments to find out more about possible side-effects. You can also read our side-effects section for more information and advice.
We're here for you
We have a range of free services for families affected by childhood cancer. Reach out to us today.
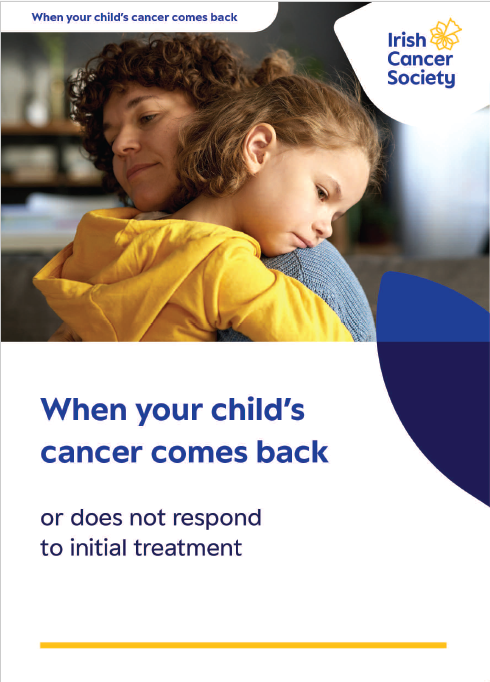
Treating cancer that comes back or isn't responding
If your child’s cancer has come back or is not responding to treatment, the treatment plan may change to slow down the growth of the cancer and reduce or relieve any symptoms.
Relapse is when cancer comes back after treatment or during treatment
Refractory cancer is cancer that is resistant to treatment
If your child’s cancer is relapsed or refractory your medical team will speak to you about what treatment options are available.
If your child’s cancer is not responding to treatment, they will be helped by the palliative care team. These are experts in treating the symptoms of advanced cancer. They will also give you emotional support.
If you want more information on symptom control and end-of-life care, please see our booklet, Precious Times.
After treatment
There's lots of things to consider after treatment including follow up care and coping with life after childhood cancer for your whole family.
We're here to help. Visit our hub for information and support on life after childhood cancer.
Are you an adolescent or young adult with cancer?
We have lots of services and information available to help you cope with a cancer diagnosis as a young person.
We're here for you
Support Line
In-hospital support